After being diagnosed with degenerative disc disease, one of the first things many patients want to know is what degenerative disc treatments are available and how doctors choose between them. Will you start with physical therapy? Are there injections that might help? How does a back and neck specialist know when it’s time to consider surgery for chronic spinal pain?
In this post, Andrew M. Davisson, MD, an interventional spine and pain specialist at Henry Community Health, explains his process and how he helps patients with disc degeneration explore care options and make treatment decisions with confidence.
“Spines are complicated. There are a multitude of things that can create pain, from issues with discs and problems in the vertebrae themselves to even arthritis. So it’s my job to hear your story, examine you, see your imaging, and figure out what’s happening to recommend the most effective treatment.”—Dr. Andrew Davisson
Keep reading for his insights about which non-surgical approaches most care plans begin with, the benefits of VIA Disc NP for patients who aren’t able to find relief from other types of conservative care, and when he recommends surgical procedures.
Non-surgical degenerative disc treatments
After a diagnosis has been confirmed, most degenerative disc care begins by exploring non-surgical options aimed at making it easier to keep active during daily life by reducing pain and improving function.
A specialist will create a custom plan, typically combining several approaches, for each patient based on factors such as symptom patterns, activity goals, work or sports demands, other health conditions, and patient preferences. “I’m always concerned with finding out each patient’s goals,” says Dr. Davisson, “because the goals of a college-age athlete are often going to be much different than, say, those of an 87-year-old woman.”
“During the first weeks of non-surgical care, I ask my patients to watch for specific milestones,” says Dr. Davisson. “I want to know if they’re noticing less stiffness when they get up from sitting, if they can do more before pain kicks in, or if their flare-ups are becoming less intense.” He explains that this sort of feedback allows him to gauge whether the current plan is working or if adjustments are needed.
The good news is that most people begin with non-surgical options (such as activity modification, physical therapy, ergonomic adjustments, medications, targeted injections, and minimally invasive procedures like VIA Disc NP), and many find significant improvements without requiring invasive surgery.
Activity modification
Making minor adjustments to your daily routine often leads to reduced pain. Breaking up long periods of sitting or standing tends to ease strain. If you’re more sedentary, gradually adding more movement to your routine generally works better than ramping up activity too quickly. Learning which activities tend to trigger degenerative disc disease flare-ups is useful for figuring out ways to avoid or modify those movements.
Physical therapy
When physical therapy is recommended for disc degeneration, the goal is to reduce pain by strengthening the muscles that support your trunk and hips (or your neck and shoulders if the disc issues you’re experiencing are in the cervical spine). Therapists work with patients to gradually build their tolerance for everyday activities, like sitting, lifting, or working at a desk.
Once patients start feeling better, the focus shifts to preventing future flare-ups. “PT helps my patients build a foundation that can prevent symptoms from recurring once they’ve found relief,” says Dr. Davisson.
Ergonomic adjustments
Your workspace and car setup might need some tweaking. Adjusting desk height can reduce strain on your back throughout the workday, and taking frequent breaks to move around can help minimize the stiffness that occurs from staying in one position for too long.
Beyond work, other ergonomic adjustments can also be beneficial. Using proper lifting techniques protects your spine from additional stress, and finding sleeping positions that keep your back or neck supported can lead to waking up with less pain.
Medications
Your doctor might suggest a short course of anti-inflammatory medication (NSAIDs like ibuprofen or naproxen) to manage pain while other treatments take effect. For patients who can’t take NSAIDs due to bleeding or gastrointestinal issues, acetaminophen (Tylenol) may be recommended as an alternative pain reliever.
The specific medicine recommended depends on what’s safe for you based on your health history and any other conditions you’re managing. These aren’t meant to be long-term solutions, so the plan includes regular check-ins to assess their effectiveness and determine if they are still needed.
Targeted injections
If your symptoms continue to limit your daily life despite trying other non-surgical approaches above, your specialist might recommend targeted pain injections.
Sometimes, when patients are in too much pain to do physical therapy, injections can be an effective way early in the treatment process to reduce pain levels enough so that you can try PT and return to day-to-day activities with greater ease.
For nerve-related symptoms (such as pain that shoots down your arm or leg), a specialist might recommend epidural steroid injections to reduce inflammation around the affected pathway. If the pain comes from a different source (like facet joint arthritis coexisting with disc degeneration), other types of image-guided injections might be more appropriate.
“My goal for patients with epidural steroid injections is 80% or more pain relief for at least six months or beyond,” says Dr. Davisson. For some patients, the relief from these injections can last one to two years or even longer. “If you’re not achieving that, then we need to kind of up the ante in terms of what we’re offering you.”
For Dr. Davisson specifically, he is only willing to continue recommending injections for patients under two conditions:
- Does the patient feel like they are helping them?
- Does his patient feel they’re worth it?
If the relief isn’t significant enough or lasts for too short a time, your specialist may recommend an alternative treatment, like VIA Disc NP.
VIA Disc NP
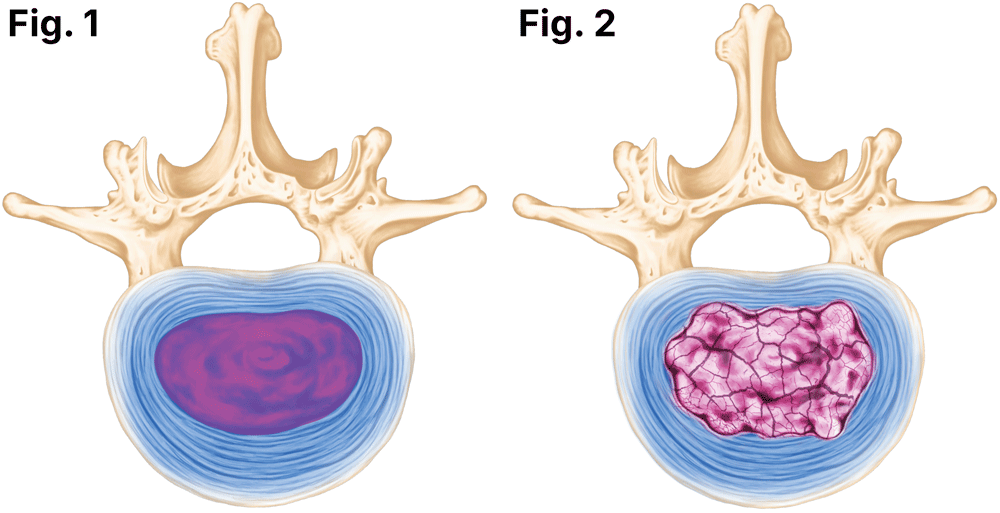
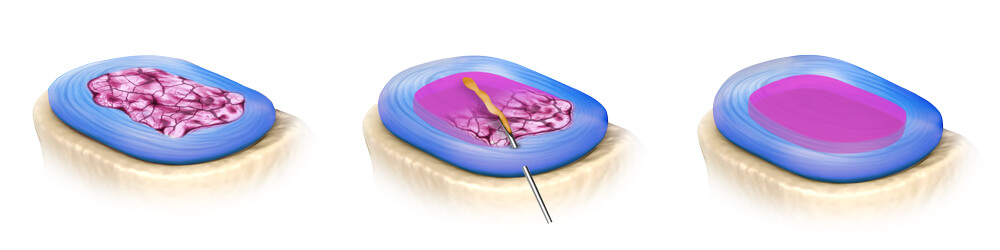
For some patients whose disc-related pain hasn’t improved with comprehensive non-surgical care, VIA Disc NP is a viable option worth considering. It’s an innovative, minimally invasive treatment that is different from traditional targeted injections for degenerating discs. “The VIA Disc NP procedure is the only treatment of its kind,” says Dr. Davisson. “It can supplement a degenerative disc with natural disc material to revitalize it.”
Rather than just managing symptoms, it solves the issue causing disc degeneration by using an allograft (a processed, natural disc material from a human donor) to rehydrate and restore tissue loss.
When talking about its benefits to patients, Dr. Davisson likes to use this analogy: “When you have a flat tire, your car won’t function right and you won’t get good gas mileage until you refill it,” he says. “You’re not going to get from point A to point B. The same is true for a degenerated disc. We can do other injections to treat the symptoms caused by disc degeneration, or we can pump up your tires by using VIA Disc NP, which will actually fix the root cause of your problem.”
Who’s a good candidate for VIA Disc NP?
A specialist considers several factors before recommending VIA Disc NP as a possible treatment option to patients with deep aching pain in the lower back from disc degeneration.
“Good candidates are people who say, primarily, ‘I have back pain,’” says Dr. Davisson. “If a patient’s primary concern is sciatica, this is not the procedure for them. VIA Disc NP is not for neuropathy. It’s not for nerve pain down your leg. VIA Disc is for chronic low back pain from degenerative disc disease that hasn’t resolved with more conservative measures.”
VIA Disc NP isn’t recommended for everyone. It’s not appropriate when there’s a suspected or confirmed infection, significant spinal instability, a large herniation with progressive neurologic loss, uncontrolled medical issues, or if someone isn’t able to participate in post-procedure activity progression.
What is it like to get a VIA Disc NP injection at HCH?
The VIA Disc NP procedure is outpatient and doesn’t take very long. “The injection only takes about five minutes,” says Dr. Davisson, who uses X-ray guidance to ensure precise placement of the allograft. “You’ll walk in and walk out the same morning. You’ll have three days of kind of taking it easy after, and then you’ll be back to your routine—even if that means you work in construction or at an assembly-line type job where you’re lifting repeatedly.”
After one injection, patients have the potential to resolve their back pain and return to full function—without needing ongoing treatments or more invasive surgery. Results are also often long-lasting, and the research findings from studies have been promising. “There’s clinical data from three to five years out showing 80% of patients won’t need a repeat VIA Disc NP injection in that time frame,” says Dr. Davisson.
HCH is one of only 20 clinical sites nationwide participating in a level one randomized controlled trial for VIA Disc NP. “Dr. Taylor and I have done more VIA Disc NP injections in our practice than any other location in the state, or—for that matter—in the Midwest,” says Dr. Davisson. “We’ve had excellent outcomes with next to no side effects or adverse events.”
Note: Although not all insurance plans currently cover the new treatment option for disc degeneration, Medicare and some commercial insurers do provide coverage for VIA Disc NP. If you’re an HCH patient, we can help verify your insurance benefits coverage and walk you through paying bills for care not covered by your plan.
Surgery
A back and neck specialist may recommend a surgical solution for treating degenerative disc disease when previous spine care hasn’t brought adequate pain relief or restored mobility. That said, most people with degenerating discs improve over time with conservative options and less invasive treatments, making surgery rarely necessary. “Surgery isn’t inevitable for patients diagnosed with disc degeneration,” says Dr. Davisson.
Spine surgery is reserved for patients experiencing progressive weakness, numbness, and coordination issues, when specific structural or neurological problems are present, or if imaging shows instability, severe disc collapse, or significant nerve compression.
Spinal fusions
Spinal fusion stabilizes painful motion at a degenerated level. Typical candidates have instability, advanced collapse with mechanical pain, or recurrent symptoms not responsive to other options. The trade-offs include reduced motion at the fused level and a possible increase in stress on nearby segments.
Artificial disc replacement
Artificial disc replacement involves using a motion-preserving implant to replace a worn disc at a single level of the spine. It’s used in carefully selected patients, more commonly in the neck and in limited cases of the lumbar spine. It’s not appropriate for patients with significant facet arthritis, osteoporosis, multi-level instability, or certain deformities.
Decompression procedures
Microdiscectomies, laminotomies, and foraminotomies are types of decompression procedures. These operations are performed to remove tissue that crowds nerves when there’s compression due to disc degeneration or other issues, such as herniation. When instability is present, a decompression procedure is sometimes paired with a spinal fusion.
Get convenient degenerative disc treatments at HCH
Good care isn’t a guess. At Henry Community Health, our experts will confirm the cause of your neck or back pain and then help you develop a personalized care plan that includes treatments to relieve your pain and increase mobility.
“Each of my patients is unique,” says Dr. Davisson. “And, every person has their own set of distinctive circumstances. The most important thing for me is really listening when they come in. I want to hear your story, learn about the nature of your pain and when it bothers you, and understand what you need and want out of treatment.”
HCH’s interventional pain management providers are leaders in the field of back and neck care. Our team offers a wide range of conservative treatments, as well as advanced solutions, such as the VIA Disc NP procedure—that often provide meaningful relief for symptoms caused by degenerative disc disease—without the need for spine surgery.
“I tell patients I’m looking to do the least amount to get you the ‘most better’ to meet your quality of life and functional goals. I’m never going to tell someone that one specific treatment is their only option.”
Don’t settle when it comes to care for your back. Schedule a consultation with our interventional spine and pain management team for comprehensive, individualized treatment that’s tailored to your specific symptoms, lifestyle, needs, and goals.
